Each year approximately 200,000 new cases of abdominal aortic aneurysms are diagnosed. Also known as AAA, an abdominal aortic aneurysm is a bulge in the aorta which could rupture with life-threatening results. Multiple studies have indicated that 5% of men and 1% of women over the age of 60 years are affected by Abdominal Aortic Aneurysms. The incidence appears to be increasing despite improved management and awareness of the disease. The experienced surgeons of Cesar Nahas MD PA are dedicated to diagnosing, managing, and treating Abdominal Aortic Aneurysms with the latest in ground-breaking medical technology and techniques.
An abdominal aortic aneurysm is the swelling or ballooning of the abdominal aorta. The aorta is the main artery that carries oxygen-filled blood from the heart to all parts of the body. In the abdomen, the aorta splits (bifurcates) into the iliac arteries, which carry blood to the legs and other lower areas of the body (see Figure 1). An aneurysm is a ballooning of the aorta which results from a weakened section in the artery that cannot support the force of blood flow (see Figure 2).
The definition of an aneurysm is a 50% increase in the diameter of an artery in comparison with its expected normal diameter. The normal size of the aorta in the abdomen is 2.5 cm (about 3/4 to 1 inch). An aorta that measures 3.75 cm or larger (about 1.5 inches) is considered to be aneurismal. Although an aneurysm can occur in any artery of the body, it is most common in the abdominal aorta and the iliac arteries. This condition, if not treated, could result in a rupture (bursting) of the aorta. The risk of rupture increases with aneurysm size and high blood pressure. Ruptured aneurysms are frequently fatal. Abdominal Aortic Aneurysms and aortic tears are the 10th leading caused of death in men ages 65-74. It is estimated that AAA causes more than 12,000 deaths annually.
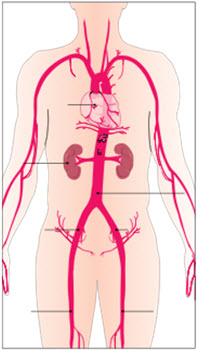
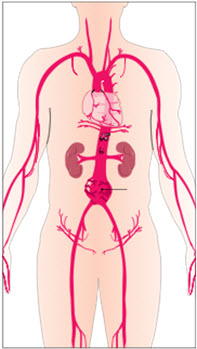
Figure 1 – The aorta is the main artery that carries oxygen-filled blood from the heart to the rest of the body. It is the largest artery in the body, extending from the chest to the abdomen where it then branches into the iliac arteries.
Figure 2 – An aneurysm is the ballooning of the abdominal aorta. The weakened sections of the aortic wall are unable to support the force of blood flow over time.
Many people do not experience any symptoms of an AAA. Because of this, it is very important to speak with your doctor about your risk of having or developing AAA disease. When symptoms do occur, pain is most commonly experienced. This can occur in the abdomen, back, or chest area. Some patients describe the pain as a mild severe pain or tenderness in the middle or upper abdomen or lower back. Other patients can feel the aneurysm as a pulsating or throbbing mass in the abdomen. Again, many people may not experience any of these symptoms, yet still be found to have an AAA.
An AAA may be discovered during a routine physical exam. Your doctor may feel a bulge or pulsation (throbbing) in your abdomen. Most often, aneurysms are found during a medical test such as a CT scan (also known as Computed Tomography or CAT scan) or ultrasound.
 Your doctor may also recommend an angiogram (see Figure 3), or additional testing such as an MRI (Magnetic Resonance Imaging)or IVUS (Intravascular Ultrasound) to determine the precise location, size, and shape of the aneurysm and your surrounding arteries.
Your doctor may also recommend an angiogram (see Figure 3), or additional testing such as an MRI (Magnetic Resonance Imaging)or IVUS (Intravascular Ultrasound) to determine the precise location, size, and shape of the aneurysm and your surrounding arteries.
Over time, the weakening of the aorta due to vascular disease, injury (trauma), or a genetic (hereditary) defect of the tissue within the arterial wall can cause an abdominal aortic aneurysm. Continuous blood pressure against this weakened area can result in the ballooning (enlarging and thinning) of the aortic artery.
Risk factors for developing an aneurysm include heredity (family history), smoking, heart disease, high blood pressure, and poor diet. Most doctors will advise simple preventative measures such as keeping your blood pressure under control, quitting smoking, and reducing cholesterol in your diet. These lifestyle changes could also aid in preventing further problems in the future. If you are at risk for developing an aneurysm, a periodic screening is recommended.
The size and location of the abdominal aortic aneurysm, and your general health, will determine how your aneurysm should be treated. When the aneurysm is small, your doctor may only recommend periodic check-ups to monitor the aneurysm. However, a larger or rapidly growing (expanding) aneurysm poses more risk of bursting (rupture), and as such, may require treatment.
Two procedural options are available:
Open surgical repair has been the traditional choice to treat abdominal aortic aneurysms. During this type of operation, the doctor makes an incision (cut) in the abdomen or side of the patient and repairs the aorta by replacing the diseased section (aneurysm) with a synthetic graft (tube) that is sewn into place with a suture. This procedure requires stopping the flow of blood through the aorta while the graft is being put into place. Open surgical repair is typically performed under general anesthesia and takes about 2 to 4 hours to complete. Patients usually stay overnight in the intensive care unit and another 5 to 7 days in the hospital. Depending on how quickly your body heals, hospitalization and recovery time may take about 3 months.
Although open repair is a proven medical procedure, not all patients can tolerate this major operation. Ask your doctor about the risks associated with an open procedure as they relate to your overall health condition.
Endovascular repair is a relatively new procedure for the treatment of abdominal aortic aneurysms. Less invasive than open surgery, it involves excluding (sealing off) the aneurysm by placing an endovascular graft inside of the diseased aorta, making a new path for the blood to flow. The endovascular graft remains inside the aorta permanently through the use of metal prongs, or anchors, as well as a tight fit (radial force) against the wall of the aorta. Endovascular repair may be performed under general, regional or local anesthesia while the patient remains conscious (awake) but sedated, and typically takes 1 to 3 hours to complete. Patients may have a hospital stay of only a few days and can usually return to normal activity within 6 weeks after the procedure.
This procedure does require routine, periodic follow-up visits with your doctor. Tests are performed to evaluate the procedure and monitor the success of the treatment. Not every patient is a candidate for endovascular repair.

 Currently, follow-up is advised to include check-ups at 1 month, 6 months, and annually thereafter. It is very important that you go to all follow-up visits recommended by your doctor.
Currently, follow-up is advised to include check-ups at 1 month, 6 months, and annually thereafter. It is very important that you go to all follow-up visits recommended by your doctor.
The follow-up exams will consist of routine X-rays, CT Scans, and a physical exam. The exams may also include blood tests, and ultrasound or MRI Scans if other imaging methods are necessary. These follow-up exams carry some minimal risk. However, the benefits of these tests clearly outweigh any potential risks.